The COVID-19 pandemic has affected more than 100 million people worldwide. Despite obvious concerns about the high mortality rate, according to a WHO report, approximately 98% of those ill survived, but survival was often associated with residual fibrotic changes in the lungs, as evidenced by chest CT scans and pulmonary function test data. Given that COVID-19 often involves severe impairment of many body organ functions, many other abnormalities may persist as the acute phase of the disease resolves, potentially affecting well-being. Various forms of pulmonary vascular involvement have been reported many times, especially in the most severe cases. Cardiac involvement has been described in a small but not insignificant proportion of patients in the acute phase of the disease.
In addition, the severe systemic inflammatory response in COVID-19 can lead to anemia, which is common in such patients and reduces the ability to carry oxygen in the blood. In addition, hospitalization for COVID-19 typically lasts several weeks, is characterized by prolonged bed rest and administration of myotoxic (muscle toxic) medications that can contribute to profound muscle dysfunction and atrophy, especially in intensive care unit patients. In addition, there has been concern that COVID-19 may be directly or indirectly associated with myopathic (myopathy – a lesion of muscle tissue) changes. However, the impact of all these multisystem changes on patients’ functional capacity at the time of discharge from the hospital after COVID-19 is still unknown.
Based on the above considerations, it has been suggested that the oragnum oxygen pathway from the beginning of inspiration to the mitochondria may be impaired at several stages (ventilation or heart pump, pulmonary circulation, blood oxygen carrying capacity, muscle ability to extract oxygen from blood) immediately after clinical resolution of COVID-19 pneumonia.
The authors of the paper, published in the Journal of Applied Physiology, sought to quantify and describe the extent and underlying mechanisms of exercise limitation in patients after hospital discharge. They did this by combining cardiopulmonary exercise with echocardiography (cardiac ultrasound) and comparing patients who were cured of COVID-19 with a matched control group. Based on analogy with previous reports of survivors of severe acute respiratory syndrome, the authors expected that COVID-19 might be associated with a decrease in exercise tolerance of about 20%.
Eighteen patients with COVID-19 and a control group were included. The groups were matched for age, sex, and BMI. All included underwent spirometry, echocardiography, stress test, and stress echocardiography to investigate pulmonary circulation. Arterial blood samples were taken at rest and during exercise in patients with COVID-19.
What were the results?
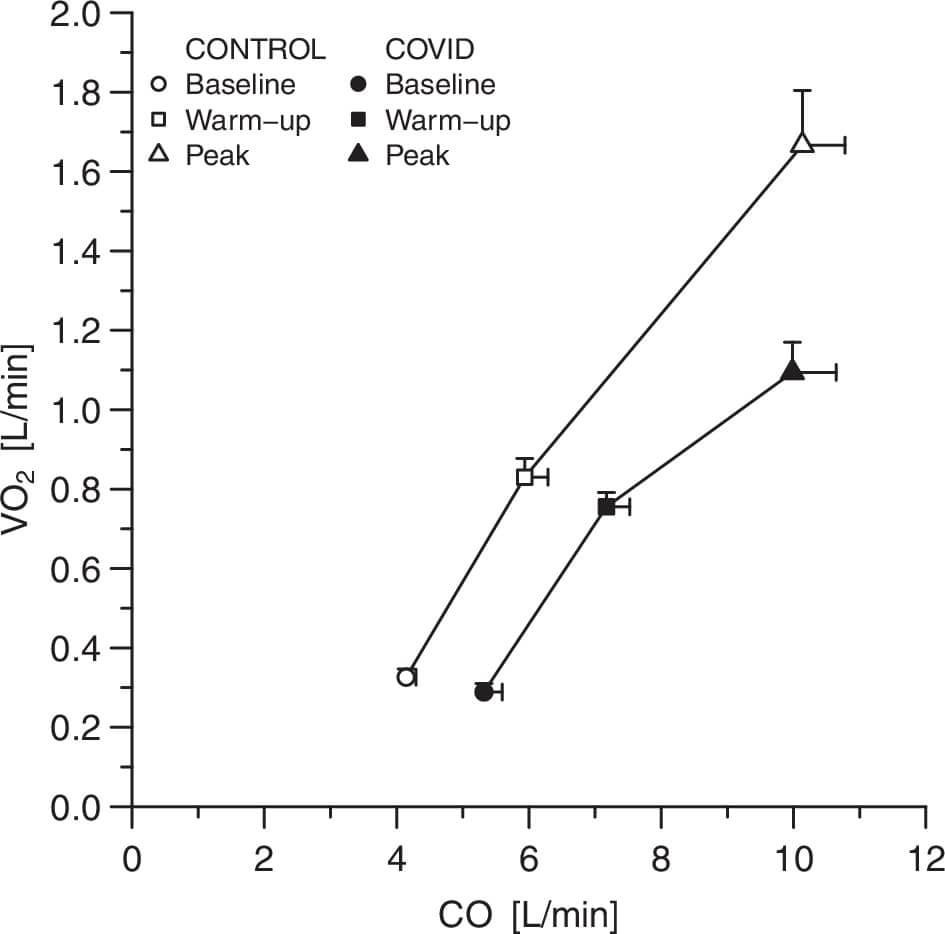
Patients with COVID-19 are on roughly the same oxygen consumption curves as the control group, both at rest and during the submaximal exercise test, due to the above-normal (that is, above-normal values) cardiac output. Oxygen consumption at maximal exercise was reduced by 30% in COVID-19 due to restriction of oxygen extraction in the periphery. In addition, hemoglobin content was associated with peak oxygen consumption in patients with COVID-19. Respiratory reserve in such patients was not exhausted, despite a moderate decrease in forced vital capacity (79 ± 40%; forced vital capacity is the amount of air that can be forcibly exhaled from the lungs after maximal deep breaths). The increase in pulmonary artery pressure during exercise did not differ between patients and controls.
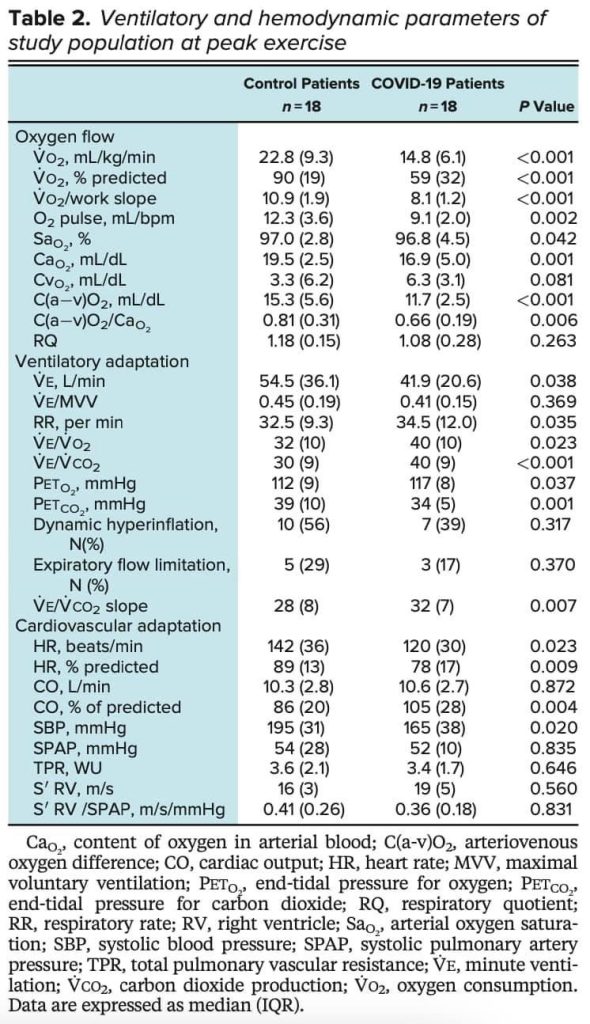
Characteristics of those included in the study
Cardiac output (X-axis) and oxygen consumption (Y-axis) in the control group (uncolored figures) and in covid patients (colored figures)
In recovery from COVID-19, patients have decreased exercise capacity and increased hyperventilation (hyperventilation is an increase in respiratory rate) during exercise. Peripheral factors, including anemia and decreased peripheral muscle oxygen extraction, were the main determinants of impaired exercise physiology despite supranormal cardiac output values. Pulmonary vascular function was not affected despite the changes in the lungs.
Leave a Reply